How should we manage hyperkalaemia?
Sep 11, 2025How do you manage the patient with hyperkalaemia? Guidelines are based on literature that is not robust.
In this review we look at the guidelines and then at some of the more recent lierature that challenges the proposed algorithms.
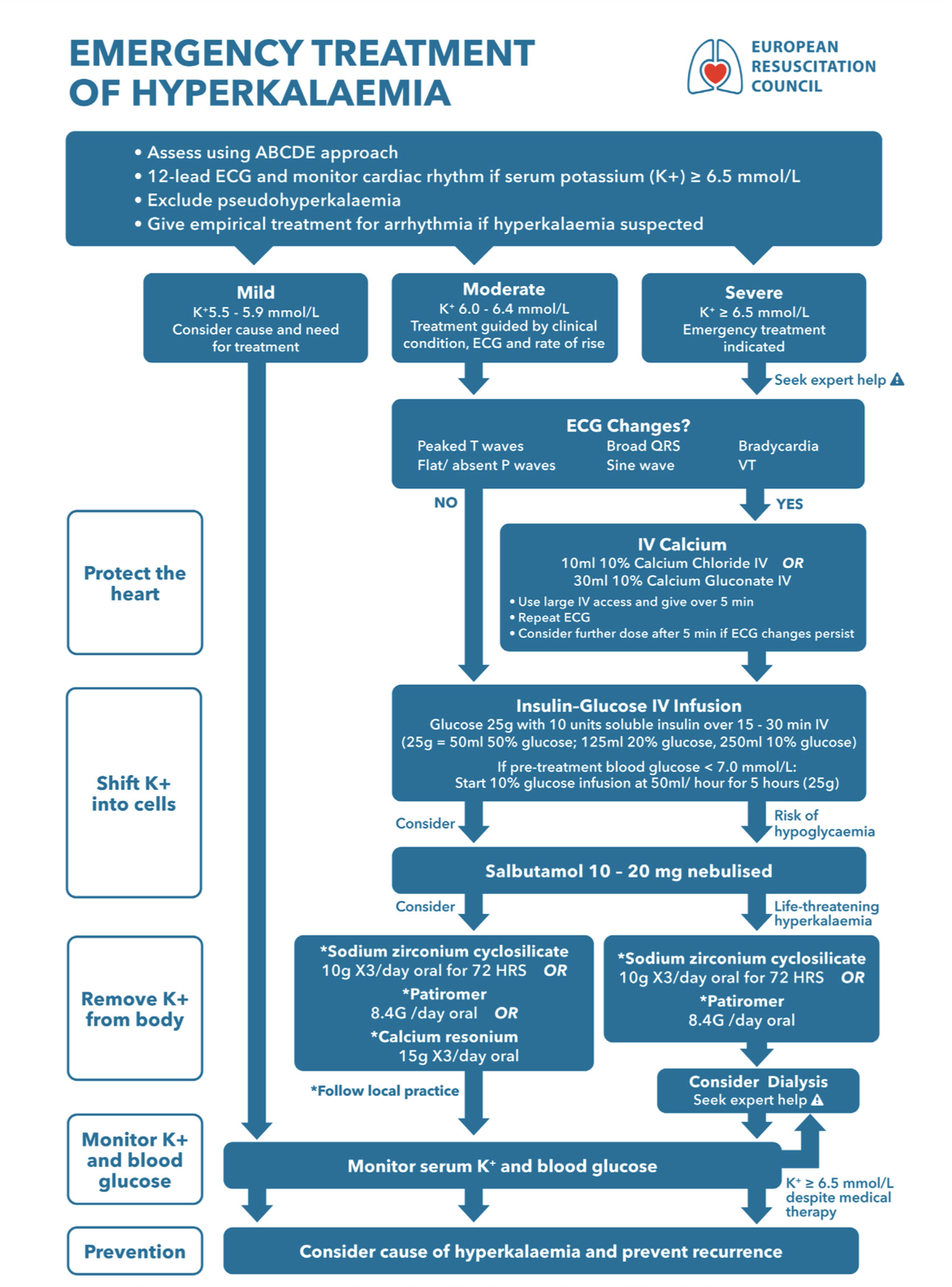
European Resuscitation Guidelines for Hyperkalaemia (1)
The goals are listed as:
- Protecting the heart: this usually involves administration of Calcium
- Shifting the potassium into the cells; usually involving glucose and insulin and salbutamol in severe cases
- Removing the potassium from the body: involves either dialysis or a binding agent, the later, which may not really have an effect in the emergency department.
- Monitoring the potassium and glucose levels.
Let's look at two groups of patients:, those in cardiac arrest from severe hyperkalaemia and those not arrested, with varying degrees of hyperkalaemia.
The Patient in Cardiac Arrest
Once the posassium level is confirmed ie., by point of care testing, or if we have a high level of suspicion ie., in a dialysis patient.
- Protect the heart: 10ml Calcium Chloride 10% IV bolus and consider repeating
- Shift Potassium into cells
- 10U Insulin and 25g (50ml of 50% or 250ml of 10%) glucose IV.
- 50mmol Sodium Bicarbonate (50ml 8.4%)
- Remove potassium from the body: consider dialysis
If the patient is Not in Cardiac Arrest
According to the guidelines, ECG changes may play a role in determining treatment. Toxic ecg changes are described in the guidelines as:
- Peaked T waves
- widened QRS
- Flat/absent P waves
- Sine Wave
- Bradycardia
- VT
The potassium levels described are:
- 5.5-5.9 mmol/l: Mild, look for causes
- 6.00-6.4 mmol/l: Moderate. The guidelines determine treatment based on the ecg
- No ECG changes: Give Glucose 25g and 10U insulin over 15-30 minutes
- ECG changes: Protect the heart first by giving 10ml Calcium Chloride or 30ml Calcium Gluconate, then add insulin and Glucose
- > 6.4 mmol/l: Severe
- No ECG changes: Add Salbutamol to insulin and Glucose. The guidelines also recommend removal of potassium from the body. Patiromer 8.4g/day oral or Resonium 15g x3/day oral
- ECG Changes: Add 10ml Calcium Chloride10% to insulin and glucose, salbutamol. The guidleines also recommend removing potassium from the body: Patiromer 8.4g/day oral or Resonium 15g x3/day oral
Below is the treatment algorithm from the ERC guidelines:
What does the literature say?
In a systematic review and meta-analysis by Jessen et al (2), 101 studies were included for review. There were limitations due to the low quality of evidence available and the fact that it included both human and animal studies. What they found was very different to what we expect:
- The use of insulin combined with glucose, beta2 agonists inhaled or intravenous (dissolved in glucose) resulted in an average reduction of potassium of 0.7 to 1.2 mmol/l.
- Bicarbonate did not really cause a change in potassium levels
- No evidence was found for a clinical benefit of calcium. This review found no evidence for its ability to prevent arrhythmias.
- Intravenous salbutamol is effective in reducing potassium.
We need to beware treating patients based on ECG changes. Studies show that 50% of patients with potassium >6.8 mom/l had ECG changes(3) ie., a normal ecg does not exclude hyperkalaemia.
A normal ecg may be associated with a lower risk of adverse events. This doesn't mean don't treat the patient, it means that we may have a little more time. Isolated peaked T waves may also be associated with a lower risk of adverse events.
Calcium itself is not without risks, the most obvious being due to extravasation, however it has been a mainstay of treatment.
Who should we give calcium to?
There is no real consensus at present. A guide may be related to the stability of the patient and the presence of ECG changes.
- Patients with mild hyperkalaemia (<6.0-6.5 mmol/L) and no ECG changes, should not receive calcium (4,5). There is some consensus here.
- There is however no real consensus about patients with hyperkalaemia (>6.0-6.5 mmol/L) with no ECG changes or with isolated peaked T waves (6)
Should we give Sodium Polystyrene Sulfonate?
These potassium-bindings resins, do not rapidly decrease the potassium levels, but lower them over several hours or days. There is little evidence to show that they are appropriate in the emergency setting(8). Use of these resins has also been associated with gastrointestinal adverse events including ulcers, colonic necrosis and perforation (9).
References
- Lott C et al. European resuscitation Council Guidelines 2021: Cardiac Arrest in Special Circumstances. Resuscitation 2021;161: 152-219
- Jessen K.K et al. Pharmacological interventions for the acute treatment of hyperkalaemia: A systematic review and meta-analysis.Resuscitation 208 (2015) 110489.
- Freeman K, et al. Effects of presentation and electrocardiogram on time to treatment of hyperkalemia. Acad Emerg Med. 2008;15:239–49.
- Alfonzo A, Soar J, MacTier R, et al. Clinical practice guidelines: treatment of acute hyperkalaemia in adults. UK Renal Assoc. 2014;147:59–77.
- Truhlář A, Deakin CD, Soar J, et al. European resuscitation council guidelines for resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201.
- Durfey N, Lehnhof B, Bergeson A, et al. Severe hyperkalemia: can the electrocardio- gram risk stratify for short-term adverse events? West J Emerg Med. 2017;18: 963–71.
- Mahoney BA, et al. Emergency interventions for hyperkalaemia. Cochrane Database Syst Rev. 2005(2):6–38 Art. No.: CD003235.
- Wu Y-H, Chou J-W, Lai H-C, Su G-S, Cheng K-S, Chen T-W. Adverse gastrointestinal effects with kayexalate or kalimate: a comprehensive review. Clin Exp Gastroenterol. 2021;14:1–18.
Join Our Free email updates
Get breaking news articles right in your inbox. Never miss a new article.
We hate SPAM. We will never sell your information, for any reason.













