The FAINT Score
Jul 23, 2025"The quest for an accurate risk-stratification tool has been the holy grail of syncope research for the last 2 decades."
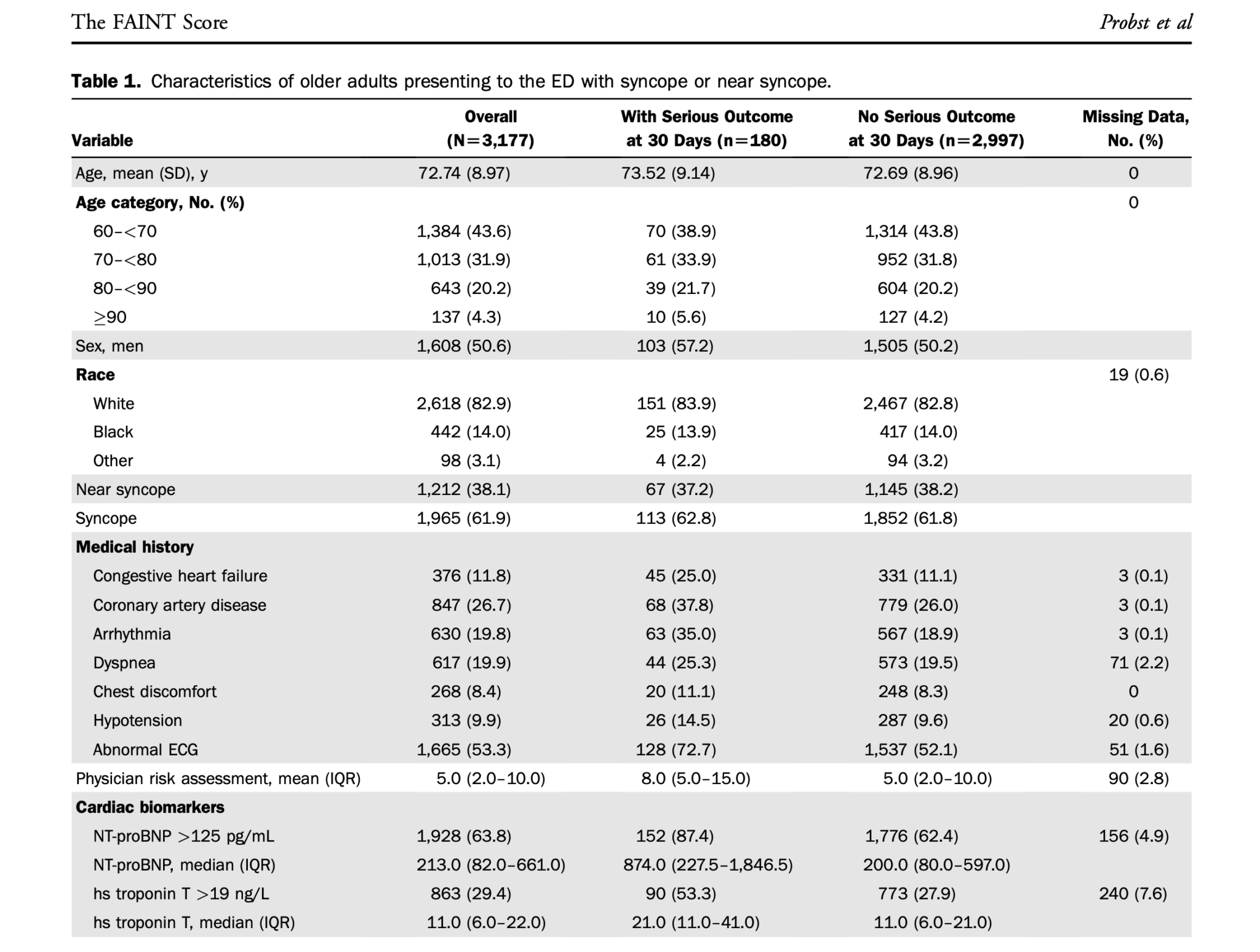
This study aimed to develop a risk-stratification tool to predict 30-day all-cause mortality and serious cardiac outcomes in older adults with a presentation of unexplained syncope or near-syncope.
The Study
Probst M A., et al. Risk Stratification of Older Adults Who Present to the Emergency department With Syncope: The FAINT Score. Ann of Emerg Med. February 2020; Vol 75, No 2. pp 147-158
What They Did
This was a multicenter, prospective, observational study. Patients > 60 years with syncope (transient loss of consciousness, associated with postural loss of tone, with immediate, spontaneous, and complete recovery) or near syncope (sensation of impending loss of consciousness without losing consciousness), were included.
All patients had a history, examination, cardiac biomarkers and a 12-lead ECG performed. Other tests were at the discretion of the treating doctor.
Physician gestalt was also assessed and the treating ED physician was asked to "estimate the probability that the patient would experience cardiac death or serious cardiac event at 30 days (0% to 100%) ".
The Primary Outcome was 30-day all-cause death or serious cardiac outcome. This included cardiac arrhythmia (eg., VT, VF, Blocks, Bradycardias, pacemaker malfunctions) myocardial infarction, a new diagnosis of structural heart disease (eg., aortic stenosis, hypertrophic cardiomyopathy or pulmonary hypertension, or cardiac intervention (pacemaker/defibrillator insertion, angioplasty, cardiac bypass).
N= 3,177
What They Found
The most common outcome was a cardiac arrhythmia, with symptomatic SVT being the most common arrhythmia found(35/180, 19.4%).
5 variables were found to be significantly associated with the Primary Outcome:
- HIstory of Heart Failure
- History of Cardiac Arrhythmia
- Abnormal Initial ECG
- Elevated NT-proBNP
- Elevated HS-cTnT level
An older patient with syncope or near-syncope with a FAINT Score of zero would be considered low risk. The risk of death or serious cardiac outcome at 30 days was considered to be:
- 0.9% (95% CI 0.3% to 1.9%) if their FAINT score was zero and
- 6.9% (95% CI 6% to 8%) if the score was greater than zero.
- Sensitivity of 96.7%
- Specificity of 22.2% and
- Positive Predictive Value of 6.9%
- Negative Predictive Value of 99.1%
The positive likelihood ratio for a FAINT score of 1 or more was 1.24 (95% CI 1.156 to 1.336) and the negative likelihood ratio was 0.15(95% CI 0.068 to 0.329).
Overall results are shown below:
The FAINT Score appeared to perform better than unstructured physician assessment. However it did not result in a significant reclassification of patients when compared to Clinician judgement.
The score failed to identify serious ourcomes in 6 patients and it would have identified 11 patitns who were not admitted as being high risk.
My Take on This.
This score specifically looked at older patients who potentially have more serious causes of syncope and near-syncope.
The score appeared to perform better than clinician gestalt, however did not really reclassify patients. It has a very low specificity for scores > zero and still needs to be externally validated.
It also uses a NT-proBNP assay and high sensitivity troponin. I think that in the older group of patients we are finding more and more that we are performing a troponin, although with no clinical reason, I would not normally perform a BNP, even though it is associated with an odds ratio of 2.5 for a serious cardiac outcome.
The score like most others should not be used as a screening tool for admission, but as a check tool before discharge. It can in fact lead to more investigations, some of which will prolong ED stay. It does one thing for me, remind me that this is a higher risk group we are dealing with and we do need to be careful.
Join Our Free email updates
Get breaking news articles right in your inbox. Never miss a new article.
We hate SPAM. We will never sell your information, for any reason.













